Hospice care team provides compassionate support, including medical, emotional, and spiritual care, ensuring comfort and dignity for patients during their end-of-life journey.
Hospice care is a distinct model of health care that aims at enhancing the quality of life based on the medical diagnosis that emphasizes terminal prognosis. Its mainstay is a committed staff of people who propagate the bodies, mind, and spirit of the patients and their dear ones. These hospitals are comprised of not only medical professionals but also end-of-life caregivers in hospice care, empowering these patients in their last moments with gentility and dignity. Knowledge of the positions within a hospice team reveals the range of development of the hospice services.
Hospice care: Looking at the principles of philosophy of care
Hospice care is founded on the understanding that the human being is a biopsychosocial and spiritual being. It focuses more on the symptomatic management and the patient’s comfort rather than the cure. This approach benefits not only the patient but also his/her family members in coming to terms with a given terminal illness.
Hospice care is based on a close-knit team of professionals with extensive experience in different aspects of end-of-life care, and one team member is always dedicated to developing an individual patient care plan that best addresses the patient’s needs, wishes, and backgrounds.
Members of the Hospice Team
1. Physicians
The hospice medical director is responsible for the medical plan of the patient to receive proper physiologic, psychological, and other medical treatments that address the patient’s pain. They are always in touch with the patient’s primary care doctor on the respective care plans and the patient’s values. They specialize in palliative medicine, which defines them to handle other condensed medical conditions with tactfulness.
2. Nurses
Hospice care is staffed by professional and paraprofessional personnel, mainly nurses who offer care and compassionate support. They prescribe medications, assess and evaluate the conditions, as well as explain to families ways of managing the children. One caring interaction involved hospice nurses developing close bonds with some of the patients to keep them warm and comfortable, especially toward the last days of their lives. Nurses also relate and connect with other members of the team to organize for changes in care as may be required.
3. Social Workers
The hospice social workers are needed to help support patients and families with the problems they may encounter on the emotional, social, and organizational levels. They give support for handling the psychological anguish arising from a terminal illness, offer information on services to be provided to the family, and support on matters like the provision of a durable power of attorney or searching for scholarships.
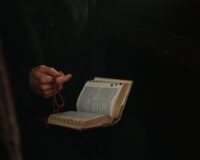
4. Chaplains/Spiritual Advisors
As in any population, spirituality or existential issues are a major concern in performing the last phase of care for many of the patients. Hospice members such as chaplains or spiritual counselors ensure that patients receive counseling that responds to their beliefs and/or their individual value systems. Their support can assist patients to find meaning within their pain and for the period of this vulnerable stage of life.
5. Bereavement Counselors
Loss doesn’t happen only at the moment of a patient’s passing but during the illness too, and far beyond it. Bereavement counselors thus assist families with feeling or dealing with grief and what life is like after losing a loved one. Usually, counseling, support groups, and community education are provided for at least a year or more after the patient has died.
6. Volunteers
This team involves the volunteers and independent practitioners, who help with company, caregiver relief, or chores within the hospice. They can add much-needed emotional reprieve and a sense of routine for both patients as well as families. Most volunteers today have firsthand experience with hospice care, which makes them very understanding.
7. Therapists and Specialists
In some instances, hospice has PT, OT, or speech therapists as members of the patient’s hospice team if the patient requires help with mobility, speaking, or performing activities of daily living. Nurses may also call an art or music therapist to offer the patient creative ways to express himself or herself or to gain comfort.
How Hospice Staff Members Interact?
The effectiveness of hospice care is best managed by its team members. All the professionals gather at the table to share their knowledge because every patient and his or her family has multiple needs covered. Such events make it easier for members of a team to discuss care plans, learn from each other, and possibly tweak certain care plans depending on the new development of the patient.
This makes the handling of patients and their families easier and watertight since they have been grouped into different categories. For example, a nurse might help manage a patient’s pain, while at the same time, a social worker addresses an accompanying emotional issue, and a chaplain works on a spiritual concern. Altogether, they make joined-up care.
Members of the Hospice Teams and Family Support
Hospice multi-professionals comprehend that terminal illness positively impacts the patient as well as his or her family members. It is understood that families receive numerous and often overwhelming emotional and practical tasks, which is why hospice care exists.
Hospice teams keep families informed of their involvement in caregiving tasks to ensure that the families are able to feel equipped when they are dealing with hospice teams. They affirm people emotionally to ensure that parents or families never feel like they are on their own. Through grief and communication, hospice teams help families begin to value whatever time is left with the dying person.
The Impact of Hospice Teams
Clearly, hospice teams’ work is not limited to the strict clinical care provided to hospice patients and their families. Both passion and love ensure that patients and families receive comfort during one of life’s hardest processes. In addition to managing pain, comforting, and providing companionship, hospice teams help patients live their last days with the most quality and integrity possible.
It is common to hear the blessings that the hospice teams themselves have brought and not only how they have cared for the patient but given support and relief to the family. The support they get assists them to come out of grief and have a sense of closure for which they are grateful.
Conclusion
Hospice teams are great examples of compassionate care. This way, they serve not only patients and their families but also change the dreadful process of terminal illness into treating it as value-based connection, care, and a worthy end. It gives patients a chance to battle the worst phase of their lives with dignity and gives families a way to come to terms with the loss. That is why hospice care has become one of the key principles of a patient-centered and collaborative approach to compassionate health services.
Looking for the Best Hospice Care of Greater Portland & Salem, OR?
At VistaRiver, we believe in providing the right care at the right time to the whole person. We guarantee a superior level of care and support for our patients and their families. If you have any questions or want to speak with someone, we’d love to hear from you. A real person will reach out to you in 24 hours! Call us at: +1 503-542-7090 or Visit: https://www.vistariver.dreamhosters.com/